KIDNEY CONNECTION: INSIGHTS INTO CHRONIC KIDNEY DISEASE MANAGEMENT FOR THE INTERDISCIPLINARY HEALTHCARE TEAM
Liz Fredrickson, PharmD, BCPS
Liz Fredrickson is an Associate Professor of Pharmacy Practice and Pharmaceutical Sciences at the Northeast Ohio Medical University College of Pharmacy. She serves as Director of Instructional Labs and is course director for the Basic Pharmaceutics Lab and Parenteral Products and Parenteral Products Lab courses.
Topic Overview
Chronic Kidney Disease (CKD) remains a significant public health problem with the evolving landscape of diagnosis, management, and patient care. As new research insights emerge and treatment paradigms shift, it is imperative for healthcare professionals to stay current with the latest recommendations and care models. This monograph will provide an overview of the management of CKD, highlighting updates from the 2022 KDIGO guidelines and focusing on updates in pharmacotherapeutics and components of comprehensive care plans.
Accreditation Statement:

RxCe.com LLC is accredited by the Accreditation Council for Pharmacy Education (ACPE) as a provider of continuing pharmacy education.
Universal Activity Number (UAN): The ACPE Universal Activity Number assigned to this activity is
Pharmacist 0669-0000-23-205-H01-P
Pharmacy Technician 0669-0000-23-206-H01-T
Credits: 1 contact hour of continuing education credit
Type of Activity: Knowledge
Media: Internet/Home study Fee Information: $4.99
Estimated time to complete activity: 1 contact hour, including Course Test and course evaluation
Release Date: December 4, 2023 Expiration Date: December 4, 2026
Target Audience: This educational activity is for pharmacists.
How to Earn Credit: From December 4, 2023, through December 4, 2026, participants must:
Read the “learning objectives” and “author and planning team disclosures;”
Study the section entitled “educational activity;” and
Complete the Course Test and Evaluation form. The Course Test will be graded automatically. Following successful completion of the Course Test with a score of 70% or higher, a statement of participation will be made available immediately. (No partial credit will be given.)
Credit for this course will be uploaded to CPE Monitor®.
Learning Objectives: Upon completion of this educational activity, participants should be able to:
Identify the latest diagnostic tools, biomarkers, and imaging techniques for early and accurate detection of chronic kidney disease (CKD)
Identify the different stages or classifications of CKD
Recall therapeutic management strategies for patients with CKD
Describe components of comprehensive care plans for patients with CKD and diabetes and patients with CKD and heart disease
Disclosures
The following individuals were involved in the development of this activity: Liz Fredrickson, PharmD, BCPS, and Pamela Sardo, PharmD, BS. Pamela Sardo was an employee of Rhythm Pharmaceuticals until March 2022 and has no conflicts of interest or relationships regarding the subject matter discussed. There are no financial relationships relevant to this activity to report or disclose by any of the individuals involved in the development of this activity.
© RxCe.com LLC 2023: All rights reserved. No reproduction of all or part of any content herein is allowed without the prior, written permission of RxCe.com LLC.
Introduction
Chronic kidney disease is a condition that poses significant challenges for patients and healthcare providers. The diagnosis and management of chronic kidney disease are guided by several clinical guidelines. Effective diagnosis and management of chronic kidney disease require clinicians to be familiar with its causes and risk factors. Treating patients with chronic kidney disease can be challenging because it can progress unnoticed during its early stages. Pharmacists and pharmacy technicians, as part of a patient’s interdisciplinary healthcare team, can provide care to improve outcomes for patients with chronic kidney disease. This monograph will review the epidemiology, etiology, pathophysiology, and risk factors associated with chronic kidney disease. Evidence-based treatment modalities, lifestyle modifications, and pharmacological interventions will also be discussed.
Defining Chronic Kidney Disease
Chronic kidney disease (CKD) is a progressive disease.1,2 There is no cure for CKD, and the disease has high morbidity and mortality, commonly in adults.2 Chronic kidney disease is more pronounced in people with diabetes and hypertension.2 Chronic kidney disease is diagnosed using the glomerular filtration rate (GFR) since it is the best indicator of kidney function. Chronic kidney disease is defined by a GFR of less than 60 mL/min/1.73 m2, albuminuria of at least 30 mg per 24 hours, or markers of kidney damage such as hematuria persisting for more than 3 months.1,2
Clinical Guidelines
The diagnosis and management of CKD are guided by several clinical guidelines, including those from KDIGO, the National Kidney Foundation (NKF), and the American College of Physicians (ACP). These are summarized in Table 1.1,3,4
Table 1
Clinical Guidelines and Recommendations for the Management of CKD
| Organization (Year) | Description |
| KDIGO (2012) | Provide comprehensive recommendations for CKD diagnosis, evaluation, and management, with a focus on evidence-based medicine |
| NKF (2022) | Offers practical tools and recommendations for the evaluation and management of CKD |
| ACP (2014) | Provide clinical recommendations for managing CKD in adults, emphasizing shared decision- making and individualized treatment plans |
Epidemiology
Chronic kidney disease rates have reached epidemic proportions, varying by region and population demographics. In the United States (US), CKD affects approximately 14% of adults, making it a significant public health concern.5 For individuals in the US, the estimated risk of developing a GFR below 60 mL/min/1.73m2 within one’s lifetime is 50%.6 Worldwide, an estimated 8-16% of the population is affected by CKD.7
Etiology
Clinicians should be familiar with the causes and risk factors associated with CKD. Determining the cause plays a vital role in selecting treatment modalities.7 Several systemic diseases can lead to CKD, including diabetes, chronic infections, and autoimmune diseases.7 Among higher-income countries, diabetes mellitus, and hypertension are leading causes, with diabetes accounting for 30-50% of cases.7,8 Apart from diabetes and hypertension, CKD can result from glomerulonephritis and or be due to genetic factors.8 Numerous factors may put individuals at risk of developing CKD.7 These are summarized in Table 2 and discussed in detail below.7
Table 2
CKD Risk Factors7
| Clinical Risk Factors |
| Diabetes |
| Hypertension |
| Autoimmune diseases |
| Systemic infections (e.g., HIV, hepatitis B virus, hepatitis C virus) |
| Nephrotoxic medications (e.g., nonsteroidal anti-inflammatory drugs, herbal remedies, lithium) |
| Recurrent urinary tract infections |
| Kidney stones |
| Urinary tract obstruction |
| Malignancy |
| Obesity |
| Reduced kidney mass (e.g., nephrectomy, low birth weight) |
| History of acute kidney injury |
| Smoking |
| Intravenous drug use (e.g., heroin, cocaine) |
| Family history of kidney disease |
| Sociodemographic Risk Factors |
| Age >60 years |
| Nonwhite race |
| Low-income |
| Genetic Risk Factors |
| APOL1 risk alleles |
| Sickle cell trait and disease |
| Polycystic kidney disease |
| Alport syndrome |
| Congenital anomalies of the kidney and urinary tract |
| Other familial causes |
Pathophysiology
Understanding the pathophysiological mechanisms of CKD is essential for effective management.8 As mentioned above, CKD is a progressive condition characterized by the gradual loss of kidney function.8 Renal fibrosis is a common pathological indicator across various CKD conditions and represents the kidney's attempt to heal itself after chronic injuries, resulting in glomerulosclerosis, tubular atrophy, and interstitial fibrosis.8 The figure
below visually depicts a nephron to guide this discussion of CKD pathophysiology.9
Nephron
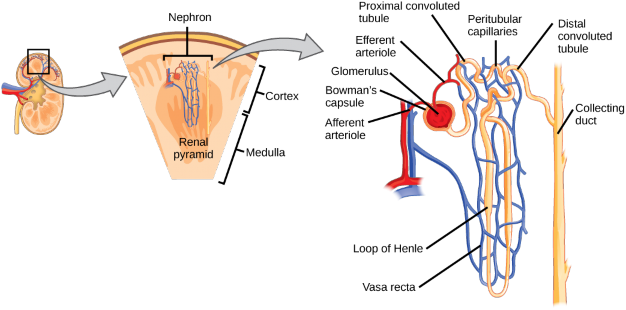
Glomerulosclerosis is inflammation and damage to the glomerulus.8 This damage is caused by endothelial damage and the proliferation of smooth- muscle and mesangial cells, which are cells responsible for the glomerular injury response.8 Simply explained, glomerulosclerosis is sclerosis (hardening/scarring) of the glomerulus, which is the initial filtering portion of the nephron. 8 Factors like hypertension, dyslipidemia, and smoking increase the risk of progressive glomerulosclerosis.8 Inflammatory responses, initiated by activated endothelial cells in response to hypertension, lead to mesangial cell proliferation. Eventually, mesangial expansion happens, which is an early sign of glomerulosclerosis. 8
Glomerular filtration rate and proteinuria are strongly related to tubular atrophy, interstitial fibrosis, and scarring.8 Tubular epithelial cells produce inflammatory substances and attract inflammatory cells into the renal interstitium.8 This process triggers interactions with interstitial myofibroblasts.8 Injured tubular epithelial cells lose their ability to regenerate
as fibrosis worsens, which leads to tubular atrophy and either dysfunctional or non-functional glomeruli.8
Additionally, the kidneys undergo interstitial capillary permeability changes in CKD, causing plasma proteins to enter the renal interstitium and cause inflammation.8 Reduced interstitial capillary surface area leads to kidney hypoxia, affecting collagen degradation, which is essential in healthy kidneys.8 Deposition of collagens, basement membrane proteins, proteoglycans, and glycoproteins occurs in the damaged kidney. The extent of fibrotic interstitium correlates with renal function and long-term prognosis.8
Staging and Classifying Chronic Kidney Disease
Chronic kidney disease is defined as the presence of abnormal kidney structure or function for at least three months.7 This can include the following: This includes 1 or more of the following: (1) GFR less than 60 mL/min/1.73 m2; (2) albuminuria (i.e., urine albumin ≥30 mg per 24 hours or urine albumin-to-creatinine ratio [ACR] ≥30 mg/g); (3) abnormalities in urine sediment, histology, or imaging suggestive of kidney damage; (4) renal tubular disorders; or (5) history of kidney transplantation.7 Staging of CKD is dependent on GFR, albuminuria, and the cause of CKD.7 Staging of GFR is as follows:1,7
G1 (GFR ≥90 mL/min/1.73 m2)
G2 (GFR 60–89 mL/min/1.73 m2)
G3a (45–59 mL/min/1.73 m2)
G3b (30–44 mL/min/1.73 m2)
G4 (15–29 mL/min/1.73 m2)
G5 (<15 mL/min/1.73 m2)
Albuminuria staging is classified as A1 (urine ACR <30 mg/g), A2 (30– 300 mg/g), and A3 (>300 mg/g).7 The classification of CKD according to international guidelines is detailed in Table 3.8
Table 3
CKD Classification per International Guidelines
GFR descriptors and range |
Range (mL/min/1·73m2) | Persistent albuminuria categories, descriptors, and ACR range | |
Normal to Moderately mildly increased increased (30– (<30mg/g) 300mg/g) | Severely increased (>300 mg/g) | ||
| G1 | Normal or high | ≥90 1 if CKD 1 | 2 |
G2 |
Mildly decreased | 60– 89 1 if CKD 1 |
2 |
G3a Mildly to moderately decreased
G3b Moderately to severely decreased
G4 Severely decreased
45–
| 1 | 2 | 3 |
| 2 | 3 | 3 |
3 |
3 | ≥4 |
| ≥4 | ≥4 | ≥4 |
59
30–
44
15–
29
G5 Kidney failure <15
Note: CKD = chronic kidney disease. GFR = glomerular filtration rate; ACR = albumin creatinine ratio. Higher frequency monitoring is recommended for those categories at most risk of progression of CKD. Small fluctuations in GFR are common. Progression is a decline in GFR of ≥25% from baseline. Factors associated with progression include cause of CKD, level of GFR, concentration of albuminuria, acute kidney injury, age, sex, race or ethnicity, raised blood pressure, hyperglycemia, dyslipidemia, smoking, obesity, history of cardiovascular disease, and ongoing exposure to nephrotoxic agents.
Clinical Presentation
Chronic kidney disease may progress silently in the early stages.8 Many patients with CKD remain asymptomatic until the disease has advanced significantly, or it is uncovered through routine laboratory testing.8 As CKD progresses, patients may develop non-specific symptoms that may be overlooked or attributed to other medical conditions.8 These can include fatigue, weakness, poor appetite, and weight loss.7 As uremic retention
products accumulate in the body, patients can experience signs and symptoms within most organ systems.8 These are detailed in Table 4.8
Table 4
Signs and Symptoms of CKD8
| Sign/Symptom | Description |
| Appearance | Pallor secondary to anemia |
| Hypertension | Primary or secondary affect |
| Shortness of breath | Due to fluid overload, anemia, or cardiomyopathy |
| Kidney issues | Kidney abnormalities dependent on cause |
| Itching and cramps | Itching due to deregulation of immune response; cramps caused by neuronal irritation |
| Cognitive changes | Language and attention affected in particular |
| Gastrointestinal symptoms | Anorexia, vomiting, taste disturbance |
| Change in urine output | Polyuria; oliguria; nocturia; anuria |
| Hematuria | Results from immune injury to glomeruli |
| Proteinuria | Due to tubular damage |
| Peripheral edema | Due to sodium retention or nephrotic syndrome |
Diagnosis
Clinical Evaluation
Early diagnosis of CKD is crucial for effective management and the prevention of complications. A comprehensive clinical evaluation is essential for CKD diagnosis. Clinicians should obtain a thorough medical history. This assists in identifying risk factors such as diabetes, hypertension, and pertinent family history. The physical examination can assess for signs of CKD, including hypertension, edema, anemia, and structural abnormalities in the kidneys. It is recommended to screen patients 60 years of age or older or those with
diabetes or hypertension.7 The following are important laboratory diagnostic tests for the diagnosis of CKD.
estimated Glomerular Filtration Rate (eGFR) eGFR is calculated using equations such as the Modification of Diet in Renal Disease (MDRD) or the 2021 Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formulas.10-12 The CKD-EPI is the most used equation.11 The 2021 CKD-EPI replaced the 2009 CKD-EPI equation because the 2009 CKD-EPI included race coefficients in its non-GFR determinants of serum creatinine.10 The use of the race coefficient was criticized since it did not perform well in non-American Blacks, and it inflated the GFR in Black patients by up to 16%.11,12 This led to poor care for these patients, leading practitioners to abandon the 2009 CKD-EPI.11,12 The 2021 CKD- EPI is race-free and creatinine-based, and its use is strongly supported by organizations and experts in this field.11,12 Estimated GFR is reported based on filtration markers, most commonly creatinine.7 Cystatin C can be used with creatinine in the CKD-EPI equation for patients with either altered creatinine production or metabolism.1,7 Table 5 provides references for the eGFR equations to keep on hand.
| Equation | Link to Source |
| Modification of Diet in Renal Disease (MDRD) | https://www.kidney.org/content/mdrd- study-equation |
| Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula | https://www.kidney.org/content/ckd-epi- creatinine-equation-2021 |
| CKD-EPI Equation | https://www.mdcalc.com/calc/3939/ckd- epi-equations-glomerular-filtration-rate-gfr |
Table 5 Estimated GFR Equations
Creatinine: Creatinine is a byproduct of muscle metabolism.7 Elevated serum creatinine levels can indicate kidney dysfunction. However, clinicians should note concentrations of creatinine also increase with
increased muscle mass and are also affected by factors including physical activity, meat intake, and creatinine degradation.8 Some medications like cimetidine can also falsely increase creatinine concentrations.8 Equations calculating eGFR use variables like age, sex, and ethnicity to handle this variability in creatinine concentrations.8
Urine Albumin-to-Creatinine Ratio (UACR): Loss of protein and albumin above the normal values for adults can be indicative of kidney disease.8 Measurement of UACR quantifies albuminuria.7,8
Kidney Imaging: Renal ultrasound is a first-line tool to assess patients yet to be diagnosed with kidney disease.8 Ultrasound can be particularly helpful in determining the cause of kidney disease.8 Other imaging modalities may include Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) but are not commonly used to diagnose CKD.8
Kidney Biopsy: Percutaneous kidney biopsy can assist clinicians in not only diagnosing CKD and its underlying cause but also determining therapies.8 It is associated with risks including bleeding or kidney damage and is only fatal in very rare cases; therefore, CKD is often diagnosed without a biopsy.8
Management
The effective management of CKD is essential to slow disease progression, alleviate symptoms, and reduce the risk of complications.
Reducing the Risk of Cardiovascular Disease
A vital part of CKD management is reducing a patient’s cardiovascular risk, given the incidence of cardiovascular disease is significantly higher in patients with CKD.7 It has been recommended that patients should receive a low-to-moderate dose statin if they are over 50.7 This is regardless of low- density lipoprotein levels.7 It is also important to promote smoking cessation and healthy lifestyles aimed at reducing cardiac risks.7
Hypertension
Per KDIGO guidelines, clinicians should target a systolic blood pressure goal of less than 120 mmHg when tolerated.1,13 Studies have found more intensive blood pressure goals are associated with lower risks of both major cardiovascular events and all-cause mortality.14 In the SPRINT (Systolic Blood Pressure Intervention Trial), individuals with an increased risk of cardiovascular disease and without diabetes targeted a blood pressure goal of below 120 mmHg systolic.14 This goal was associated with a 25% lower risk of major cardiovascular events and a 27% reduction in all-cause mortality compared to the group with a targeted systolic blood pressure of below 140 mmHg.14 However, the group with the more intensive blood pressure target also had a larger risk of experiencing a 30% or more decline in eGFR, to a level below 60 mL/min/1.73m2.14

The pharmacologic management of hypertension involves the use of angiotensin-converting enzyme inhibitors (ACE-I) or angiotensin II receptor blockers (ARBs).7,13 Angiotensin-converting enzyme inhibitors and ARBs control blood pressure and have direct reno-protective effects by reducing proteinuria and slowing the progression of CKD.7 These agents are beneficial for patients with diabetes and a urine ACR of minimally 30 mg per 24 hours or adults with a urine ACR of 300 mg per 24 hours. Angiotensin-converting enzyme inhibitors and ARBs should not be used concurrently due to hyperkalemia and acute kidney injury risk.7 For patients with hypertension, the primary goal of their use is to control blood pressure, and a secondary
goal is to control proteinuria.15 For patients with albuminuria, resistant hypertension, or heart failure with reduced ejection fraction, aldosterone receptor antagonists may be started.7 Angiotensin-converting enzyme inhibitors and ARB dosing are presented in Table 6. Creatinine and potassium levels should be monitored when initiating or titrating these therapies.16-20
Table 6
ACE-I and ARB Drug Dosing16-20
| Medication | Dosing |
| Lisinopril | 2.5 to 10 mg once daily: titrate to response up to 40 mg/day |
| Captopril | 25 mg 3 times daily; titrate to goal blood pressure and proteinuria goal |
| Enalapril | 2.5 mg – 5 mg in 1-2 divided doses. Titrate to tolerability and response up to 40 mg daily in 1-2 divided doses |
| Losartan | 25-50 mg once daily. Increase up to 100 mg once daily based on blood pressure and tolerability |
| Valsartan | 40-80 mg twice daily. Titrate up to 160 mg twice daily based on BP response and tolerability. |
Diabetes Mellitus
The management of diabetes mellitus is also a crucial component of CKD management.7 Managing diabetes is multifactorial. The 2020 KDIGO Diabetes Management in CKD guidelines recommend treating patients with a comprehensive care plan to reduce their risk of both kidney and cardiovascular disease progression.21 First, patients should aim to obtain a goal hemoglobin A1C (A1C) level of approximately 7%.21 This A1C level is recommended per multiple guidelines. Second, various diabetic medications may need to be dose-adjusted depending on the level of kidney disease present.7 Medications such as the sulfonylurea glyburide, which is mainly cleared by the kidneys, should be avoided.7
Finally, clinicians should consider utilizing sodium glucose transport-2 inhibitors (SGLT-2) inhibitors in patients with highly increased albuminuria.7 These agents reduce glucose and sodium reabsorption in the proximal tubule of the kidney, decrease glomerular hyperfiltration, and reduce glomerular hypertension.15 The efficacy of this was demonstrated in the Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation (CREDENCE) trial.22 In this trial, patients who had type 2 diabetes and CKD stage G2-G3/A3 (baseline eGFR 30 to <90 mL/min/1.73 m2 and urine ACR>300 to 5000 mg/24 hours) and who were taking an ACE-I or ARB and canagliflozin had a 30% lower risk of doubling their serum creatinine, developing end-stage kidney disease, or experiencing death from a renal or cardiovascular cause.22 Once an SGLT-2 inhibitor is started, it should be continued until dialysis or kidney transplantation.22
Dietary Management
The role of dietary interventions in the context of slowing CKD progression is unclear. Some studies have found that while a low protein diet compared to a normal protein diet eventually slowed GFR decline, the effects of a very low protein diet were no different compared to a low protein diet.23,24 Per the KDIGO guidelines, patients with stage G4 or G5 CKD should work with a dietician to establish a diet with a protein intake of less than 0.8 mg/kg/day.1 Patients at risk of CKD progression should reduce protein intake to less than
1.3 mg/kg/day.1 Other dietary recommendations involve the inclusion of fruits, vegetables, and fiber within the diet and limiting eggs, meat, and cheese.7 Sodium should be limited to less than 2 grams per day.1,15
Medication Considerations
Pharmacists can assist the care team in identifying nephrotoxins and counseling patients to avoid medications deemed nephrotoxic, meaning they can harm kidneys. There are numerous medications considered nephrotoxins. Some of these include:
Non-steroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs should be avoided in CKD, especially if the patient is also taking ACE inhibitors (ACE-I) or Angiotensin Receptor Blockers (ARB) therapy.7
Herbal products: Herbal medications are especially concerning, given they are not regulated by the Food and Drug Administration (FDA). Some products, such as those containing aristolochic acid or anthraquinones, can lead to serious issues, including acute tubular necrosis and nephrolithiasis.7
Phosphate-based bowel preparations: These preparations, including both oral and enema forms, can cause acute phosphate nephropathy.7
Proton pump inhibitors (PPIs): Proton pump inhibitors use has been linked to acute interstitial nephritis and CKD in some cases.7 It is important for healthcare providers to work with patients to determine if their need for continued PPI use is warranted a primary care visits.
Outside of avoiding nephrotoxic medications, clinicians should also ensure every medication taken is dose-adjusted for renal function if necessary. Several commonly prescribed medications, including antibiotics, direct oral anticoagulants, gabapentin, pregabalin, oral hypoglycemic agents, insulin, chemotherapeutic drugs, and opiates, often need dose reductions in CKD patients to prevent adverse drug events.7 It is advisable to limit the use of medications with low expected benefits in CKD patients due to their increased risk of side effects. Gadolinium-based contrast agents should be avoided in individuals with acute kidney injury, eGFR less than 30 mL/min/1.73 m2, or end-stage kidney disease due to the risk of nephrogenic systemic fibrosis, a painful condition causing skin and organ fibrosis.7 Newer formulations of gadolinium are less likely to cause this condition, but it's best to avoid gadolinium when possible.7 If necessary, patients should be informed about the potential risk, and consultation with a nephrologist for postexposure hemodialysis may be considered.
Managing CKD Complications
Anemia
Anemia is a common complication of CKD. Anemia is the result of reduced erythropoietin production, and management involves the use of iron supplementation and erythropoiesis-stimulating agents (ESAs).7 The KDIGO guidelines recommend initiating ESA therapy when hemoglobin levels fall below 10 g/dL.1 However, ESA therapy should be used judiciously, balancing the benefits of improved quality of life and reduced transfusion requirements with potential risks, such as increased cardiovascular events.25
Bone and Mineral Disorders
In one study of CKD patients, 58% had parathyroid hormone (PTH) levels above 65 pg/mL.26 Management of CKD bone and mineral disorders includes optimizing calcium and phosphate levels, controlling PTH, and addressing vitamin D deficiency.7 Phosphate binders and active vitamin D analogs are commonly used to manage CKD-MBD.7
Nephrology Referral
Timely referral to a nephrologist is essential, especially for patients with advanced CKD (Stage 4 or 5). Nephrologists can provide specialized care, assess the need for renal replacement therapy (dialysis or transplantation), and offer guidance on complex management decisions.
Renal Replacement Therapy (RRT)
For patients with end-stage renal disease (ESRD), renal replacement therapy options include hemodialysis, peritoneal dialysis, and kidney transplantation.7 Transplantation is the preferred option when feasible, offering a better quality of life and improved survival compared to dialysis.27
Monitoring CKD
Per KDIGO, eGFR, and albuminuria should be monitored at least once annually.1 High-risk patients should be monitored twice per year or more.7 Very high-risk patients should be monitored at least 3 times per year.7 An individualized approach to CKD is recommended. Drugs that act directly on the renin-angiotensin system can cause injury and death to the developing fetus and should be avoided in pregnancy. If a pharmacy technician notices a prescription or over-the-counter purchase of prenatal vitamins with an ACE inhibitor or ARB prescription, the pharmacist should be notified. CKD is complex, and an unmet medical need to optimize outcomes remains. In a non- diabetic African American population with a GFR of 20–65 mL/ min/1.73 m2 randomized to control BP with follow-up of 3+ years, only patients with baseline proteinuria>1 g/day demonstrated slowing of CKD with intensive blood pressure control.28
The Role of Pharmacy Staff
Pharmacists involved in medication therapy management can be effective members of the interdisciplinary health team for treating patients with CKD.29 In outpatient primary care, pharmacists may help improve proteinuria screening and CKD management.29
Pharmacy technicians play important roles on the healthcare team with regard to patients with CKD.30 As the practice of pharmacy evolves, pharmacy technicians are beginning to assist with and perform nontraditional functions.30 In dialysis units, pharmacy technicians may perform medication reconciliation and medication management services. This aids the healthcare team in optimizing care for these high-risk patients.
Additionally, it is important for patients to tell their pharmacist and provider about all medications they are taking. Pharmacy technicians may notice a patient has a prescription or over-the-counter purchase of potassium or an NSAID and can notify the pharmacist.
Key Take-Away Considerations
Because patients with CKD often have complex medication regimens, pharmacy teams are optimally positioned to review the patient record for drug interactions and possible dose adjustments. As discussed, laboratory monitoring is also important. Pharmacists can reinforce adherence to drug therapies and provide patient education. Counseling on healthy lifestyle habits may include eating a low-salt diet, lower protein intake, or eliminating alcoholic beverages. Medication reconciliation and disease management discussions with multidisciplinary care teams can optimize patient care. Motivational interviews should emphasize taking medications as directed to control blood pressure, weight, and plasma glucose.
Summary
Chronic kidney disease is an increasingly prevalent condition that poses significant challenges for patients and healthcare providers. The growing burden of CKD underscores the urgency of equipping healthcare professionals with the most up-to-date knowledge and strategies for effectively managing this condition. Recent advancements within nephrology and a growing body of knowledge have provided valuable insights into the early detection, risk stratification, and therapeutic interventions for CKD. Pharmacists can best care for their patients by having a comprehensive understanding of CKD, including its underlying causes and approaches to diagnosis and treatment. Pharmacy technicians may perform medication reconciliation and medication management services.
Course Test
Which diagnostic test is essential for CKD diagnosis and staging?
Estimated glomerular filtration rate
Blood pressure measurement
Urine color
X-ray of the kidneys
What is the primary test used to detect albuminuria?
Serum creatinine
eGFR
Urine albumin-to-creatinine ratio (UACR)
Kidney ultrasound
Which imaging technique is commonly used to assess kidney structure and determine the cause of CKD?
MRI
CT scan
Renal ultrasound
X-ray
What is the recommended systolic blood pressure goal for CKD patients according to KDIGO guidelines?
<120 mmHg
<130 mmHg
<140 mmHg
<160 mmHg
Which class of medications is recommended for the management of hypertension in CKD patients, especially those with albuminuria?
Beta-blockers
ACE inhibitors or ARBs
Calcium channel blockers
Diuretics
What is the recommended target hemoglobin A1C level for CKD patients with diabetes?
<6%
<7%
<8%
<9%
Dieticians can assist patients with CKD to reach their care goals. Which dietary recommendation is appropriate for CKD patients to help slow disease progression?
High-protein diet
Low-sodium diet
High-fat diet
Low-fiber diet
What is a key component of managing bone and mineral disorders associated with CKD?
Reducing protein intake
Controlling parathyroid hormone (PTH) levels
Achieving hypercalcemia
Avoiding vitamin D supplementation
Clinicians should consider the use of which of the following medications in patients with CKD, diabetes, and greatly increased albuminuria?
metformin
sulfonylureas
sodium-glucose transport-2 inhibitors
meglitinides
Which of the following types of products are not regulated by the Food and Drug Administration and should be avoided in patients with CKD?
NSAIDs
ACE-inhibitors
Herbal supplements
Diabetic medications
References
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3(1):1– 150
Kalantar-Zadeh K, Jafar TH, Nitsch D, Neuen BL, Perkovic V. Chronic kidney disease. Lancet. 2021;398(10302):786-802. doi:10.1016/S0140-6736(21)00519-5
NKF KDOQI Clinical Practice Guidelines. National Kidney Foundation. 2022. https://www.kidney.org/kidney-basics. Accessed November 13,
2023.
Qaseem A, Hopkins RH Jr, Sweet DE, Starkey M, Shekelle P; Clinical Guidelines Committee of the American College of Physicians. Screening, monitoring, and treatment of stage 1 to 3 chronic kidney disease: A clinical practice guideline from the American College of Physicians. Ann Intern Med. 2013;159(12):835-847. doi:10.7326/0003-4819-159-12- 201312170-00726
Chronic Kidney Disease in the United States, 2023. Centers for Disease Control and Prevention. 2023. https://www.cdc.gov/kidneydisease/publications-resources/ckd- national-facts.html. Accessed November 13, 2023.
Grams ME, Chow EK, Segev DL, Coresh J. Lifetime incidence of CKD stages 3–5 in the United States. Am J Kidney Dis. 2013;62(2):245–252. doi: 10.1053/j.ajkd.2013.03.009
Chen TK, Knicely DH, Grams ME. Chronic Kidney Disease Diagnosis and Management: A Review. JAMA. 2019;322(13):1294-1304. doi:10.1001/jama.2019.14745
Webster AC, Nagler EV, Morton RL, Masson P. Chronic Kidney Disease. Lancet. 2017;389(10075):1238-1252. doi:10.1016/S0140- 6736(16)32064-5
WikiCommons. Nephron. https://commons.wikimedia.org/wiki/Category:Nephron#/media/File:Fi gure_41_03_03.png. Accessed November 13, 2023.
Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate [published correction appears in Ann Intern Med. 2011 Sep 20;155(6):408]. Ann Intern Med. 2009;150(9):604-
612. doi:10.7326/0003-4819-150-9-200905050-00006
Zingano CP, Escott GM, Rocha BM, et al. 2009 CKD-EPI glomerular filtration rate estimation in Black individuals outside the United States: a systematic review and meta-analysis. Clin Kidney J. 2022;16(2):322-
330. Published 2022 Oct 29. doi:10.1093/ckj/sfac238
Tsai JW, Cerdeña JP, Goedel WC, et al. Evaluating the Impact and Rationale of Race-Specific Estimations of Kidney Function: Estimations
from U.S. NHANES, 2015-2018. EClinicalMedicine. 2021;42:101197.
Published 2021 Nov 19. doi:10.1016/j.eclinm.2021.101197
Armstrong C; Joint National Committee. JNC8 guidelines for the management of hypertension in adults. Am Fam Physician. 2014;90(7):503-504.
Wright JT Jr, Williamson JD, Whelton PK, et al.; SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2103–2116. doi: 10.1056/NEJMoa1511939
Wazny LD. Chronic Kidney Disease. In: DiPiro JT, Yee GC, Haines ST, Nolin TD, Ellingrod VL, Posey L. eds. DiPiro’s Pharmacotherapy: A Pathophysiologic Approach, 12th Edition. McGraw Hill; 2023
Zestril. Prescribing information. Astra Zeneca Pharmaceuticals LP. December 2014. https://www.accessdata.fda.gov/drugsatfda_docs/label/2014/019777s0 64lbl.pdf. Accessed November 25, 2023.
Capoten. Prescribing information. Par Pharmaceutical Companies, Inc. June 2012. https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/018343s0 84lbl.pdf. Accessed November 25, 2023.
Vasotec. Prescribing information. Valeant Pharmaceuticals North America LLC. August 2015. https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/018998s0 80lbl.pdf. Accessed November 25, 2023.
Cozaar. Prescribing information. Merck & Co., Inc. March 2013. https://www.accessdata.fda.gov/drugsatfda_docs/label/2013/020386s0 58lbl.pdf. Accessed November 25, 2023.
Diovan. Prescribing information. Novartis Pharmaceuticals, Corp. January 2017. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/021283s5 0lbl.pdf. Accessed November 25, 2023.
Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Work Group. KDIGO 2020 Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease. Kidney Int. 2020;98(4S):S1- S115. doi:10.1016/j.kint.2020.06.019
Perkovic V, Jardine MJ, Neal B, et al. Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. N Engl J Med. 2019;380(24):2295-2306. doi:10.1056/NEJMoa1811744
Klahr S, Levey AS, Beck GJ, et al.; Modification of Diet in Renal Disease Study Group. The effects of dietary protein restriction and blood- pressure control on the progression of chronic renal disease. N Engl J Med. 1994;330(13):877–884. doi: 10.1056/NEJM199403313301301
Robertson L, Waugh N, Robertson A. Protein restriction for diabetic renal disease. Cochrane Database Syst Rev. 2007;(4):CD002181.
Palmer SC, Navaneethan SD, Craig JC, et al. Meta-analysis: erythropoiesis-stimulating agents in patients with chronic kidney disease. Ann Intern Med. 2010;153(1):23-33. doi:10.7326/0003-4819- 153-1-201007060-00252
Inker LA, Grams ME, Levey AS, et al.; CKD Prognosis Consortium. Relationship of estimated GFR and albuminuria to concurrent laboratory abnormalities: an individual participant data meta-analysis in a global consortium. Am J Kidney Dis. 2019;73(2):206–217. doi: 10.1053/j.ajkd.2018.08.013
Hart A, Lentine KL, Smith JM, et al. OPTN/SRTR 2019 Annual Data Report: Kidney. Am J Transplant. 2021;21 Suppl 2:21-137. doi:10.1111/ajt.16502
Wright JT Jr, Bakris G, Greene T, Agodoa LY, Appel LJ, Charleston J, et al. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial. JAMA. 2002;288:2421–31.
Chang AR, Evans M, Yule C, et al. Using pharmacists to improve risk stratification and management of stage 3A chronic kidney disease: a feasibility study. BMC Nephrol. 2016;17(1):168. Published 2016 Nov 8. doi:10.1186/s12882-016-0383-7
Codd C, Martinusen D, Cardone KE, Cho K, Pai AB. Preparing for implementation of a medication reconciliation measure for dialysis: Expanding the role of pharmacy technicians. Am J Health Syst Pharm. 2020;77(11):892-896. doi:10.1093/ajhp/zxaa077
DISCLAIMER
The information provided in this course is general in nature, and it is solely designed to provide participants with continuing education credit(s). This course and materials are not meant to substitute for the independent, professional judgment of any participant regarding that participant’s professional practice, including but not limited to patient assessment, diagnosis, treatment, and/or health management. Medical and pharmacy practices, rules, and laws vary from state to state, and this course does not cover the laws of each state; therefore, participants must consult the laws of their state as they relate to their professional practice.
Healthcare professionals, including pharmacists and pharmacy technicians, must consult with their employer, healthcare facility, hospital, or other organization, for guidelines, protocols, and procedures they are to follow. The information provided in this course does not replace those guidelines, protocols, and procedures but is for academic purposes only, and this course’s limited purpose is for the completion of continuing education credits.
Participants are advised and acknowledge that information related to medications, their administration, dosing, contraindications, adverse reactions, interactions, warnings, precautions, or accepted uses are constantly changing, and any person taking this course understands that such person must make an independent review of medication information prior to any patient assessment, diagnosis, treatment and/or health management. Any
discussion of off-label use of any medication, device, or procedure is informational only, and such uses are not endorsed hereby.
Nothing contained in this course represents the opinions, views, judgments, or conclusions of RxCe.com LLC. RxCe.com LLC is not liable or responsible to any person for any inaccuracy, error, or omission with respect to this course, or course material.
© RxCe.com LLC 2023: All rights reserved. No reproduction of all or part of any content herein is allowed without the prior, written permission of RxCe.com LLC.
