RECENT ADVANCES IN GENE THERAPY FOR HEMOPHILIA
SALAM KADHIM, PhD
Salam Kadhim is a pharmaceutical scientist with experience in drug discovery and developing small molecule compounds, biologics, siRNA, and cannabinoids in oncology, HBV, cardiovascular, ocular, and neurodegenerative disorders.
Pamela Sardo, PharmD, BS
Pamela Sardo, PharmD, BS, is a freelance medical writer and licensed pharmacist in 3 states. She is the founder and principal at Sardo Solutions in Texas. Pam received her BS from the University of Connecticut and her PharmD from the University of Rhode Island. Pam’s career spans many years in retail, clinics, hospitals, long-term care, Veterans Affairs, and managed health care responsibilities across various therapeutic classes and disease states.
Topic Overview
Hemophilia is one of the most common serious congenital clotting-factor deficiencies. Multiple new drugs have been FDA-approved to treat hemophilia. Pharmacy team members need to be aware of the causes, treatment, and pharmacology and understand that advancements in research are generating a more patient-specific approach to care. Hemophilia treatments are becoming more patient-specific. This course provides insights into the definition of hemophilia, its types, causes, symptoms, diagnosis, and current treatment options. The focus is on the available and emerging gene therapy strategies for hemophilia. The course will address efficacy, safety, and the current challenges posed by new gene therapy pharmacological approaches. Future gene therapy applications in hemophilia are also discussed.
Accreditation Statement:

RxCe.com LLC is accredited by the Accreditation Council for Pharmacy Education (ACPEⓇ) as a provider of continuing pharmacy education.
Universal Activity Number (UAN): The ACPE Universal Activity Number assigned to this activity is
Pharmacist 0669-0000-23-144-H01-P
Pharmacy Technician 0669-0000-23-145-H01-T
Credits: 1 hour of continuing education credit
Type of Activity: Knowledge
Media: Internet/home study Fee Information: $4.99
Estimated time to complete activity: 1 hour, including Course Test and course evaluation
Release Date: September 12, 2023 Expiration Date: September 12, 2026
Target Audience: This educational activity is for pharmacists.
How to Earn Credit: From September 12, 2023, through September 12, 2026, participants must:
Read the “learning objectives” and “author and planning team disclosures;”
Study the section entitled “educational activity;” and
Complete the Course Test and Evaluation form. The Course Test will be graded automatically. Following successful completion of the Course Test with a score of 70% or higher, a statement of participation will be made available immediately. No partial credit will be given.
Credit for this course will be uploaded to CPE Monitor®.
Learning Objectives: Upon completion of this educational activity, participants should be able to:
Provide an overview of hemophilia types and characteristics
Describe the diagnosis for hemophilia
Describe the current treatment options for hemophilia
Describe pharmacological gene therapy approaches for hemophilia
Discuss current challenges in gene therapy for hemophilia.
Disclosures
The following individuals were involved in developing this activity: Salam Kadhim, PhD, and Pamela Sardo, PharmD, BS. Pamela Sardo was an employee of Rhythm Pharmaceuticals until March 2022 and has no conflicts of interest or relationships regarding the subject matter discussed. There are no financial relationships relevant to this activity to report or disclose by any of the individuals involved in the development of this activity.
© RxCe.com LLC 2023: All rights reserved. No reproduction of all or part of any content herein is allowed without the prior, written permission of RxCe.com LLC.
Introduction
Hemophilia is a hemorrhagic disease characterized by a deficiency in blood clotting. It results from gene mutations in the genes that encode clotting factor proteins that form blood clots. The disease manifests itself in excessive and prolonged periods of external and internal bleeding. The conventional hemophilia treatment replaces missing blood clotting factors through intravenous infusion of plasma and cryoprecipitates (plasma-derived) and recombinant clotting factor concentrates. While these agents and treatments are effective, the current gene therapy strategies may offer new alternatives to the replacement protocols. Recent gene therapy directions, including viral, non-viral, and gene-editing technologies, are often more effective and provide new therapeutic avenues for routine hemophilia treatment.
Definition and Prevalence of Hemophilia
Hemophilia is an inherited genetic disorder that impairs the body’s ability to form blood clots.1 It affects people from all racial and ethnic groups but is most common in males and less frequent in females.2 The two main types of hemophilia, types A and B, are X-chromosome-linked. Being X- chromosome-linked refers to characteristics influenced by genes on the X- chromosome. Hemophilia types A and B are caused by mutations in the F8 and F9 genes. This mutation results in missing or reduced production or function of clotting factor VIII (FVIII or F8) for hemophilia A and clotting factor IX (FIX or F9) for hemophilia B.3 The current global incidence of hemophilia A is estimated at 1:5,000 and hemophilia B at 1:30,000 male live births.4 The third type, hemophilia C, is a rare autosomal disorder due to factor FXI deficiency and in the US, it is thought to affect 1 in 100,000 of the adult population.5 It is important for pharmacists to have a strong foundation in the medications used to treat this condition for clinical team discussions and shared decision-making.
Hemophilia may be severe, moderate, or mild based on the amount of clotting factor in the blood. The disease severity in hemophilia A and B is classified according to the plasma levels of FVIII and FIX activity. The severe
form is defined as a factor level less than 1 IU/dL of normal, the moderate form is 1 to 5 IU/dL, and the mild form is between 5 and 40 IU/dL.6
Patients with severe hemophilia frequently develop hemorrhages in their joints, muscles, or soft tissues without an apparent cause, called spontaneous hemorrhages or bleeding. Hemophiliacs can also suffer life-threatening bleeding episodes (e.g., intracranial hemorrhages). Patients with mild and moderate factor deficiency rarely experience spontaneous hemorrhages, and excessive bleeding mostly occurs only following trauma or in association with invasive surgical procedures.
Causes of Hemophilia
Hemophilia is caused by inherited genetic mutations, mainly affecting males. The assembly of the enzyme-activated FIX encoded by the F9 gene with its cofactor, activated FVIII encoded by the F8 gene is a crucial event in the coagulation cascade needed to form a blood clot. The absence or dysfunction of either enzyme or cofactor severely compromises hemostasis and causes hemophilia.7 Hemophilia A and B are inherited in the same way since F8 and F9 mutated genes are located on the same X chromosome. The
X chromosome contains several genes that are not present on the Y chromosome. There are no genes for clotting factors on the Y chromosome.2
Males (XY) only have one allele for FVIII and one allele for FIX with both recessive genes on their X-chromosome and are termed hemizygous. Therefore, males can have hemophilia if they inherit an affected X chromosome with a gene mutation for either factor. Females (XX) carry two alleles for X-chromosome genes and are termed heterozygous. Women can be hemophiliacs but it is rarer for them. In such cases, both X chromosomes are affected, or one is affected and the other is missing or inactive. A female with one affected X chromosome is a “carrier” of hemophilia. Female carriers can have hemophilia symptoms like males; however, they have enough clotting factors from their one normal gene to prevent serious bleeding. Females can pass the affected X chromosome with the mutation to their
children. The chances of a child inheriting hemophilia depend on which of the parents has the mutated gene.
Takeaway message to ponder:
A female is believed to be a hemophilia carrier and is pregnant or considering pregnancy. How could a conversation begin regarding genetic counseling or genetic testing to confirm or rule out being a hemophilia carrier?
Symptoms of Hemophilia
The main symptom of hemophilia is bleeding. A person with hemophilia can have internal and external bleeds. External bleeds occur in the mouth, after biting the mouth, lips, or tongue, or as recurrent, heavy nosebleeds (epistaxis) without apparent cause. Also, people with external bleeds experience minor cuts that do not clot, or clot briefly and then resume bleeding.8
Internal bleeds most frequently occur in the knee, ankle, elbow, hip joints, soft tissues, and brain following trauma or during invasive surgery. Bleeds can also occur in the large muscles, such as the iliopsoas muscle in the front of the hip, causing abdominal, hip, or back pain. Symptoms of internal bleeding in women include long, heavy menstrual bleeding (menorrhagia), flooding or gushing of blood, and cramps. Large bruises can result from soft tissue bleeds under the skin.8 Mild cases may not be detected until later in life, after excessive bleeding following surgery or injury.9 People with severe hemophilia can have serious bleeding problems right away that can occur for no obvious reason. Without treatment, they can develop joint deformities, which may require joint replacement surgery, soft tissue bleeding, or serious internal bleeding.
Increased frequency of spontaneous bleeding contributes to iron deficiency and is common among patients with hemophilia.10,11 Iron deficiency adversely affects wound healing, immunity, and mental well-being. Identifying iron deficiency and treating it in these patients might improve a patient’s quality of life.10
Diagnosis of Hemophilia
Clinical diagnosis is initially made by evaluating the patient’s medical history, bleeding symptoms, physical examination, bleeding assessment tool (BAT), and family history. Diagnosis and specific laboratory tests identify coagulation factors, clotting time, and their levels in plasma. Direct sequencing of coagulation F8 or F9 genes has increased the sensitivity of screening techniques and is currently the gold standard for molecular genetic analysis of hemophilia. Including next-generation sequencing (NGS) in the routine diagnostic algorithm (screening tests and clotting factor tests) improved molecular testing in terms of speed, costs, and efficiency.12
Conventional Treatment for Hemophilia
Hemophilia treatment depends on the type and severity of the disease and includes medicines and factor replacement therapy. Off-label use of drugs is discussed below. Please refer to the official prescribing information for each product for a discussion of approved indications, contraindications, and warnings.
Traditionally, the gold standard treatment is replacing the missing clotting factor with intravenous infusion either as prophylaxis or episodically.13 Medicines to treat hemophilia include clotting factor products and several other treatment medications.
There are two main types of clotting factor concentrates. First, there is plasma derived from human plasma proteins, which are pathogen-free clotting proteins made as freeze-dried concentrate. Second, there are recombinant
factors produced by recombinant DNA technology. Recombinant factors produced by recombinant DNA technology include the following:
Octocog alfa is an engineered version of FVIII, commonly used for prophylaxis, on-demand, or during surgery. It was effective for the prevention and treatment of bleeding episodes.14 It is also called antihaemophilic factor, plasma/albumin free method, and is a recombinant, human, full-length coagulation factor VIII that does not contain human- or animal-derived plasma proteins.14 The most common treatment-emergent adverse events are pyrexia and headache. Serious adverse events include the development of high-titer factor VIII inhibitors (usually in previously untreated patients) and hypersensitivity reactions. It is administered by slow IV injection or IV infusion.
Nonacog alfa is an engineered version of FIX, commonly used for prophylaxis of hemophilia B. It is available in 250 IU, 500 IU, 1000 IU, 2000 IU, and 3000 IU, and indicated in adults and children with hemophilia B for on-demand, perioperative use, or prophylaxis of bleeding episodes. Hypersensitivity or allergic reactions have been observed and may proceed to anaphylaxis. It is administered intravenously after reconstitution with sterile solvent for injection.15
Recombinant FVIII-Fc fusion protein conjugated to polyethylene glycol with enhanced pharmacokinetic properties. Reduce the frequency of dosing. It is available nominally as 250, 500, 750, 1000, 1500, 2000, or 3000 IU, as a lyophilized powder in single-use vials for reconstitution. It is utilized for on-demand, perioperative use, or prophylaxis of bleeding episodes. The most frequently occurring adverse reactions in clinical trials were arthralgia, malaise, myalgia, headache, and rash.16
Other Treatment Products
There are several other treatments for hemophilia.
Hemlibra (ACE910, Emicizumab-kxwh) is a bispecific factor IXa- and factor X-directed antibody indicated for routine prophylaxis to prevent or reduce the frequency of bleeding episodes in adult and pediatric
patients ages newborn and older with hemophilia A (congenital factor VIII deficiency) with or without factor VIII inhibitors.17 The recommended loading dose is 3 mg/kg by subcutaneous injection once weekly for the first 4 weeks, followed by a maintenance dose of 1.5 mg/kg once every week, 3 mg/kg once every two weeks, or 6 mg/kg once every four weeks.17 The most common adverse reactions (incidence ≥10%) are injection site reactions, headache, and arthralgia. Immunogenicity and Laboratory Coagulation Test Interference are also possible. 17
Concizumab is a humanized IgG4 monoclonal antibody selective for the second Kunitz domain of tissue factor pathway inhibitor (TFPI). It restores thrombin generation by mitigating TFPI effect on the coagulation system. It is approved in Canada but is not FDA-approved in the USA.18
DDAVP or Stimate (Desmopressin Acetate) is a synthetic hormone- releasing factor FVIII from body tissues. Desmopressin acetate injection, 4 mcg/ml, is indicated for patients with hemophilia A with factor VIII coagulant activity levels >5%.19 It will often maintain hemostasis during surgical procedures and postoperatively when administered 30 minutes prior to procedures.19 It will also stop bleeding in patients with spontaneous or trauma-induced injuries.19 Very rare cases of hyponatremia have been reported. Headache, nausea, abdominal cramps, erythema, or facial flushing may occur.19
Amicar (Epsilon, Aminocaproic acid) interferes with the ability of plasmin to lyse fibrin clots. Used for treatment of acute bleeding in the mouth or following tooth extraction, or in transfusion or surgical complications.20 The FDA-approved indication does not mention hemophilia.
Fitusiran is an antithrombin RNA interference molecule that decreases antithrombin mRNA expression in the liver. It is under development and is not FDA-approved.
Antifibrinolytic agents e.g., tranexamic acid, are used to treat bleeding after childbirth or during dental work procedures. Tranexamic acid is indicated in patients with hemophilia for short-term use (2 to 8 days) to reduce or prevent hemorrhage and reduce the need for replacement therapy.21 Before extraction, administer 10 mg/kg of actual body weight
of tranexamic acid I.V. with replacement therapy.21 After extraction, administer 10 mg/kg of actual body weight 3 to 4 times daily for 2 to 8 days.21 Infuse no more than 1 mL/minute to avoid hypotension and reduce the dosage in patients with renal impairment.21 The most common adverse reactions are nausea, vomiting, diarrhea, allergic dermatitis, giddiness, hypotension, and thromboembolic events.21
Birth control pills have been prescribed to treat heavy menstrual bleeding; however, there is no indication for treating hemophilia in the prescribing information. Immunosuppressive medicines, such as prednisone, help block the production of antibodies in acquired bleeding disorders. Vitamin K supplements treat vitamin K deficiency bleeding. These have been used in clinical settings but are not FDA-approved for hemophilia.
Gene Therapy of Hemophilia
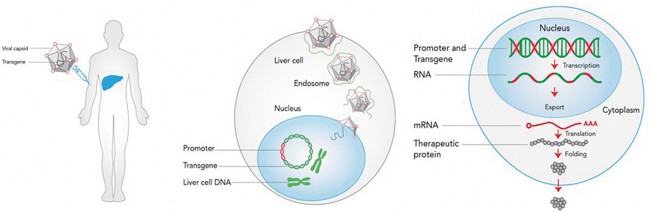
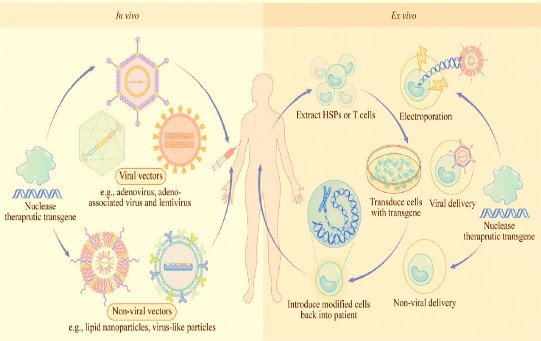
Genes may be absent or non-functional. Gene therapy can repair genes or provide a functional copy of a gene.22,23 Treating genetic diseases with gene therapy requires transgene encoding, wherein a protein is delivered to the tissue in a stable manner, without interfering with the tissue or cell integrity.24,25 The principle of gene therapy in hemophilia is to introduce an intact copy of the FVIII/FIX gene via a delivery vehicle into somatic cells, compensating for the defective gene. Hemophilia is an ideal target for gene therapy due to its monogenic nature of inheritance and since correction of a single gene can provide significant symptomatic relief.24 Gene therapy of hemophilia for transgene delivery includes viral, non-viral, physical methods, polymer-based procedures, and gene editing. Currently, the most widely used method with the potential to cure hemophilia is the viral-mediated delivery (e.g., adeno-associated, lentiviral, or gene editing) of a transgene encoding either FVIII or FIX protein. Gene therapy protocols are applied to somatic cells either in vivo, where gene correction or its insertion into cells is performed in the body through a vector; or ex vivo where the same procedure is carried out of the body in cells previously harvested from the patient then reimplanted following expansion and selection process.23,26
Targeted Gene Therapy
Pipe, et al., 202227 (open access)
Viral Vectors
Adeno-associated vector (AAV) is currently the most advanced form of gene therapy for hemophilia A and B that provides multi-year therapeutically relevant FVIII and FIX activity and clinical benefit.28-30 Adeno-associated vectors deliver coagulation factor genes directly into liver hepatocytes, which are converted to protein bio-factories, producing and secreting transgene products into circulation. The ClinicalTrials.gov31 database presently lists 18 active clinical trials evaluating different AAV-F9 capsid serotypes and gene sequences for hemophilia B and 21 trials evaluating AAV-F8 gene therapy for hemophilia A, with some overlap, as the same vectors being evaluated in both phase 1/2 and 3 clinical trials.32,33 Most of these studies, using AAV vectors with various gene constructs, show sufficient factor FVIII and FIX expression in patients to significantly reduce the number of bleeds and the need for prophylaxis.31 The AAVs efficient gene delivery, inability to integrate into the patient’s genome, and low immunogenicity make them the lead candidate for clinical gene therapy.30,,34-36 It is the best approach for liver-directed delivery of F8 or F9 genes and can potentially cure hemophilia after a single peripheral vein infusion.28,37 The two most recently approved AAV gene therapies in the EU and USA, respectively are:
Valoctocogene roxaparvovec (Roctavian, BMN-270, Valrox) is an adeno- associated virus vector-based gene therapy indicated for the treatment of adults with severe hemophilia A (congenital factor VIII deficiency with factor VIII activity < 1 IU/dL) without pre-existing antibodies to adeno- associated virus serotype 5 detected by an FDA-approved test.38 It is a suspension for intravenous infusion. The recommended dose of Valoctocogene roxaparvovec is 6 × 1013 vector genomes (vg) per kg of body weight.38 Start the infusion at 1 mL/min. If tolerated, the rate may be increased every 30 minutes by 1 mL/min up to a maximum rate of 4 mL/min.38 The most common adverse reactions (incidence ≥ 5%) were nausea, fatigue, headache, infusion-related reactions, vomiting, and abdominal pain. For 6 months after administration, men must not donate semen, and men and their female partners must prevent or postpone pregnancy.38
Etranacogene dezaparvovec-drlb (Hemgenix) consists of an adeno- associated viral vector carrying the gene for clotting factor FIX given as a one-time, single dose by IV infusion.39 It is indicated for the treatment of adults with hemophilia B (congenital Factor IX deficiency) who use Factor IX prophylaxis therapy, have current or historical life-threatening hemorrhage, or have repeated, serious spontaneous bleeding episodes.39 The recommended dose is 2 x 1013 genome copies (gc) per kilogram (kg) of body weight (or 2 mL/kg body weight) administered as an IV infusion after dilution with 0.9% sodium chloride solution.39 Patients may experience infusion reactions, hepatotoxicity, hepatocellular carcinogenicity, or immune-mediated neutralization of the AAV5 vector capsid.39 The most common adverse reactions (incidence ≥5%) reported in clinical studies were liver function test elevations, headache, blood creatine kinase elevations, flu-like symptoms, infusion-related reactions, fatigue, and malaise.39
Lentiviral vectors are emerging as powerful and versatile delivery vehicles for liver-directed gene therapy in hemophilia, achieving optimal FVIII and FIX expression in the liver.40 The vectors are based on replication- defective single-stranded RNA lentiviruses such as HIV and do not induce an immune response. Lentiviral vectors integrate into the DNA of both non-
dividing and dividing cells either ex vivo or in vivo;23,41 however, they may induce oncogenesis.42,43
Non-Viral Vectors
Non-viral vectors can circumvent some of the problems associated with viral gene delivery, including transient gene expression, integration into the host genome, adverse immune reactions, and potential hepatotoxicity. Recent advances in vector technology have made nonviral gene therapy approaches particularly appealing for hemophilia.
Liposomes are spherical-shaped small vesicles created from cholesterol and natural non-toxic phospholipids. Due to their size, biocompatibility and hydrophobic/hydrophilic properties liposomes are promising systems for gene delivery. Gene delivery via liposomes has advantages such as low immunogenic response and a large capacity for loading DNA. The lipids forming outer lipoplexes including cationic, anionic, neutral, or mixed types provide stability to the liposome-encapsulated DNA.44 Liposomes have progressed from research to clinical trials and are currently utilized in gene therapy to treat diseases such as cystic fibrosis sickle cell anemia, immune system deficiencies. The use of liposomes coupled to a human hFIX plasmid in experimental models achieved detectable hFIX expression in the liver, spleen, and plasma.45 Pegylated liposomes are being investigated for use in hemophilia to extend dosing interval and enhance potency but are not FDA approved.46
Polymers
Biodegradable polymers coupled to DNA improve gene transfer due to low toxicity and high biocompatibility. Chitosan, a polycationic gene carrier derived from a substance found in the outer shell of crustaceans, effectively binds to DNA and confers partial protection of DNA from nucleases.47 Topically available, a sterile chitosan-based dressing is available for use for the external temporary control of severely bleeding wounds and is intended for emergency use.48 Oral administration of chitosan-DNA nanoparticles is a non-invasive
option for gene delivery. Ingested DNA enters the cells in the intestinal epithelium, where the transgene is expressed.47 Therapeutic levels of hFIX in the circulation are detectable in experimental models after oral administration of chitosan nanoparticles containing hFIX plasmid.49
Protective, interactive, noncondensing (PINC) delivery systems are non-ionic polymers based on poly-L-glutamate.50 PINC may improve transgene expression in part by increasing plasmid retention in skeletal muscle.48,50 Intramuscular injection of PINC-formulated hFIX DNA in experimental models of hemophilia B achieved sustained levels of hFIX.51
Physical Methods
Delivery of DNA by direct injection of naked plasmid DNA without a carrier is one of the safest gene therapy approaches.52 Several delivery methods can be utilized including electroporation (EP), sonoporation, microinjection, particle bombardment (gene gun), and hydrodynamic injection.53 In experimental models of hemophilia A and B persistent and high levels of FIX and FVIII gene expression in livers were achieved using direct injection of naked plasmid DNA.54
Gene Editing
Gene editing is a recent technology that allows genetic material to be added, removed, or altered in the cell or organism at specific locations in the genome. In vivo delivery vehicles include viral and non-viral vectors and nanoparticles that can be loaded with the genome editor and then injected into the patient either systemically, which results primarily in liver editing, or into a specific site of interest. Ex vivo hematopoietic stem cells (HTP) or T cells can be extracted from the patient or donor, modified in the laboratory, and infused back into the patient.
Ex vivo and In vivo Strategies for Therapeutic Gene Editing
Li, et al., 202255 (open access)
Several gene-editing techniques currently in use include the following:
CRISPR/Cas9 contains two parts: “CRISPR” (Clustered Regularly Interspaced Short Palindromic Repeats) targeting genomic sequences and Cas9 a CRISPR-associated (Cas) endonuclease enzyme, which acts as “molecular scissors” to cut DNA at a location specified by a guide RNA.56,57
Transcription Activator-like Effector Nucleases (TALENs) and Zinc Finger Nucleases (ZFNs).57
siRNA (small interference RNA) intended to modify the translation of mRNA inhibiting or modifying production of the protein without affecting the encoding gene.58
While several approaches for gene editing have emerged in hemophilia treatment, the use of ZFNs is the furthest in development.59,60 A Phase 1 study in patients with severe hemophilia B is currently ongoing to assess safety, tolerability, and long-term expression of FIX by intravenous treatment with
ZFN therapeutic SB-FIX delivered via AAV-derived vector.61 The SB-FIX functions by placing a corrective copy of the FIX transgene into the genome of the subject’s hepatocytes under the control of highly expressed endogenous albumin locus, thereby providing a permanent, liver-specific expression. A Phase 1 study with fitusiran, an RNA interference (RNAi) therapy targeting antithrombin in hemophilia A and B patients, resulted in lower antithrombin levels and increased thrombin generation.62 CRISPR/Cas9 has recently progressed to the clinical stage for treating blood disorders such as β- thalassemia and sickle cell disease and is likely to be pursued for hemophilia, but no human clinical trials have emerged.63,64
Challenges of Gene Therapy
There are challenges to gene therapy for hemophilia. Potential adverse effects and challenges of hemophilia gene therapy include the following:
High administration frequency of prophylaxis regimens to achieve long coagulation factor half-live, robust efficacy, and safety profiles.65
Liver toxicity (hepatotoxicity) associated with viral and non-viral vector delivery.38,66,67
Loss or reduction of transgene expression; e.g., expression levels of FVIII decrease over time with intra- and inter-patient variability, particularly in children.67
Immunogenicity induction of humoral and T-cell immunity results in vector neutralization and reduction of treatment efficacy.68
Endogenous presence of transgene product inhibitors in patients previously exposed to AAV F8 and F9 genotypes.27
Risks of increasing frequency of off-target gene editing.66,69
Risk of genomic insertional mutagenesis/oncogenesis and infusion- related adverse reactions after gene transfer.66
Patient Counseling
There are challenges and risks to gene therapy for hemophilia. Patients need to be counseled on these subjects and their questions answered through
interprofessional collaboration. Some of the topics that patients should be educated on include the following:70
Pre-infusion blood tests will be necessary for some hemophilia treatments
There is a risk of developing neutralizing antibodies (inhibitors) to factor VIII; patients should inform clinicians if usual dosages of factor VIII are not able to control bleeding
Patients should inform clinicians if symptoms of low-grade fever, drowsiness, chills, runny nose, rash, arthralgias, arthritis, or joint pain are present
Inform clinicians if symptoms of hepatitis A infection (e.g., low-grade fever, anorexia, nausea, vomiting, fatigue, jaundice, dark urine, abdominal pain) occur
Patients should discontinue therapy and immediately inform clinicians if hives, urticaria, chest tightness, dyspnea, faintness, hypotension, wheezing, or other manifestations of hypersensitivity reaction or anaphylaxis occur
Inform clinicians of concomitant therapy, including prescription and OTC drugs, and any concomitant illnesses.
With some treatments, physician consultation is recommended because patients should not donate blood, organs, tissues, or cells for transplantation
Women should inform their clinician if they are or plan to become pregnant or plan to breast-feed
Future Trends in Gene Therapy
Improved gene delivery systems are necessary before gene therapy becomes a routine clinical approach for hemophilia patients.71,72 Safety is a particular concern in the design of novel gene therapy vectors. Future gene replacement therapies must meet the challenges of providing safe and prolonged durability of transgene expression and enhanced efficacy. Further understanding of gene regulation and expression at the cellular and molecular level would lead to developing next-generation gene transfer, vector designs,
and gene editing tools. Gene editing provides patients with hemophilia options that were not available before. The ultimate goal of hemophilia treatment would be to advance gene therapy to clinical trials and eliminate the need for exogenous plasma-derived or recombinant coagulation factors. Hemophilia patients would be cured by achieving normal hemostasis to lead normal lives without requiring intervention.
Summary
Gene therapy is a new, effective, long-term treatment option for hemophilia. The goal is to reduce bleeding episodes and reduce the number of infusions. Gene therapy can avoid the complications of other therapies. Ultimately, the patient may have better health outcomes and quality of life.
Significant clinical benefit has been accomplished in patients with hemophilia A and B with intravenously administered AAV-based liver-directed gene therapy. Sustained FVIII and FIX levels close to the normal range have been achieved, and, in most patients, prophylaxis to prevent bleeding could be discontinued or limited.
Course Test
What causes hemophilia A?
Mutation in the F8 gene
Mutation in the F9 gene
Mutation in both F8 and F9 genes
Excessive bleeding
What causes hemophilia B?
Mutation in the F8 gene
Mutation in the F9 gene
Mutation in both F8 and F9 genes
Excessive bleeding
Which of the following is a common symptom of mild hemophilia?
Hemochromatosis
Spontaneous bleeding
Hypertension
Hemorrhages
What is currently the most advanced form of gene therapy for hemophilia A and B?
Adeno-associated vector therapy
Non-viral vector therapy
Gene editing
CRISPR/Cas9
Which of the following is not a gene therapy vector?
Adeno-associated vector
Liposome vehicle
CRISPR/Cas9
Polymer carrier
Which of the following treatments for hemophilia are derived from human plasma proteins?
Desmopressin Acetate
Fitusiran
Pathogen-free clotting proteins (freeze-dried concentrate)
Tranexamic acid
Which of the following gene therapies does not involve gene editing but is delivered physically, by direct injection?
CRISPR/Cas9
Naked plasmid DNA
Zinc Finger Nuclease
siRNA (small interference RNA)
What are the potential adverse effects of hemophilia gene therapy?
Middle ear infection
Increases in F18 or F19 factors
A decrease in the frequency of off-target gene editing
Liver toxicity
The disease severity in hemophilia A and B is classified by
the white blood cell count.
the plasma levels of FVIII and FIX activity.
whether the treatment is prophylactic or episodic.
the number of blood donations to patients with type O blood.
Which of the following is not a physical method for DNA delivery?
Microinjection
Particle bombardment (gene gun)
Electroporation
Non-viral vectors (e.g., liposomes)
References
BLEEDING DISORDERS What Are Bleeding Disorders. National Heart, Lung, and Blood Institute. Published March 24, 2022. https://www.nhlbi.nih.gov/health/bleeding-disorders. Accessed January 3, 2023.
Hemophilia. Centers for Disease Control and Prevention. Published August 1, 2022. https://www.cdc.gov/ncbddd/hemophilia/diagnosis.html. Accessed January 3, 2023.
Mancuso ME, Mahlangu JN, Pipe SW. The changing treatment landscape in haemophilia: from standard half-life clotting factor concentrates to gene editing. The Lancet. 2021;397(10274):630-640. doi:10.1016/S0140-6736(20)32722-7
Lippi G, Favaloro EJ. Gene therapy for hemophilias: the end of phenotypic testing or the start of a new era? Blood Coagulation & Fibrinolysis. 2020;31(4):237-242. doi:10.1097/MBC.0000000000000905
Wheeler AP, Gailani D. Why factor XI deficiency is a clinical concern. Expert Rev Hematol. 2016;9(7):629-637. doi:10.1080/17474086.2016.1191944
Blanchette VS, Key NS, Ljung LR, Manco-Johnson MJ, van den Berg HM, Srivastava A. Definitions in hemophilia: communication from the SSC of the ISTH. Journal of Thrombosis and Haemostasis. 2014;12(11):1935- 1939. doi:10.1111/jth.12672
Freato N, Ebberink EHTM, van Galen J, et al. Factor VIII–driven changes in activated factor IX explored by hydrogen-deuterium exchange mass spectrometry. Blood. 2020;136(23):2703-2714. doi:10.1182/blood.2020005593
Types of Bleeds. Wayback Machine, National Hemophilia Foundation. Published February 13, 2010. https://www.hemophilia.org/bleeding- disorders-a-z/overview/types-of- bleeds?menuid=191&contentid=382&rptname=bleeding. Accessed January 3, 2023.
Benson G, Auerswald G, Dolan G, et al. Diagnosis and care of patients with mild haemophilia: practical recommendations for clinical management. Blood Transfus. 2018;16(6):535-544. doi:doi: 10.2450/2017.0150-17
Rae C, Furlong W, Horsman J, et al. Bleeding disorders, menorrhagia and iron deficiency: impacts on health-related quality of life. Haemophilia. 2013;19(3):385-391. doi:10.1111/hae.12014
Poongavanam P, Nandakumaran J, Shanmugam M, Pachuau H. The Frequency of Iron Deficiency among Patients with Hemophilia. IOSR-J of
Dental and Med Sciences. 2017;16(6):4-9. doi: 10.9790/0853- 1606080409
Bastida J, González-Porras J, Jiménez C, et al. Application of a molecular diagnostic algorithm for haemophilia A and B using next- generation sequencing of entire F8, F9 and VWF genes. Thromb Haemost. 2017;117(01):66-74. doi:10.1160/TH16-05-0375
Berntorp E, Fischer K, Hart DP, et al. Haemophilia. Nat Rev Dis Primers. 2021;7(1):45. doi:10.1038/s41572-021-00278-x
Dhillon S. Octocog alfa, antihaemophilic factor (recombinant), plasma/albumin free method (Advate®): a review of its use in the management of patients with haemophilia A. Drugs. 2012;72(7):987- 1007. doi: 10.2165/11207480-000000000-00000
BeneFIX®. Prescribing information. Pfizer. June 2022. https://labeling.pfizer.com/ShowLabeling.aspx?id=15011. Accessed September 1, 2023.
ELOCTATE®. Bioverativ Therapeutics Inc. May 2023. https://products.sanofi.us/Eloctate/Eloctate.pdf. Accessed September 10, 2023.
Hemlibra®. Prescribing information. Genentech, Inc. March 2023. https://www.gene.com/download/pdf/hemlibra_prescribing.pdf. Accessed September 4, 2023.
Smith, T. FDA Rejects Concizumab for Prophylactic Treatment of Hemophilia A, B. HCPLive. May 5, 2023. https://www.hcplive.com/view/fda-rejects-concizumab-prophylactic- treatment-hemophilia-a-b. Accessed September 4, 2023.
DDAVP injection. Prescribing information. sanofi-aventis, US, LLC. July 2007. https://products.sanofi.us/ddavp_iv/ddavp_iv.pdf. Accessed
September 4, 2023.
Aminocaproic acid. Hemophilia News Today. 2023. https://hemophilianewstoday.com/aminocaproic-acid/. Accessed September 4, 2023.
Cyklokapron. Prescribing information. Pfizer. March 2021. https://labeling.pfizer.com/ShowLabeling.aspx?format=PDF&id=556. Accessed September 4, 2023.
Perrin GQ, Herzog RW, Markusic DM. Update on clinical gene therapy for hemophilia. Blood. 2019;133(5):407-414. doi:10.1182/blood-2018-07- 820720
Anguela XM, High KA. Entering the Modern Era of Gene Therapy. Annu Rev Med. 2019;70(1):273-288. doi:10.1146/annurev-med-012017- 043332
Lisowski L, Staber JM, Wright JF, Valentino LA. The intersection of vector biology, gene therapy, and hemophilia. Res Pract Thromb Haemost. 2021;5(6). doi:10.1002/rth2.12586
Marchesini E, Morfini M, Valentino L. Recent Advances in the Treatment of Hemophilia: A Review. Biologics. 2021;Volume 15:221-235. doi:10.2147/BTT.S252580
High KA, Roncarolo MG. Gene Therapy. New England Journal of Medicine. 2019;381(5):455-464. doi:10.1056/NEJMra1706910
Pipe SW, Gonen-Yaacovi G, Segurado OG. Hemophilia A gene therapy: current and next-generation approaches. Expert Opin Biol Ther. 2022;22(9):1099-1115. doi:10.1080/14712598.2022.2002842
Nathwani AC. Gene therapy for hemophilia. Hematology. 2019;2019(1):1-8. doi:10.1182/hematology.2019000007
George LA, Sullivan SK, Giermasz A, et al. Hemophilia B Gene Therapy with a High-Specific-Activity Factor IX Variant. New England Journal of Medicine. 2017;377(23):2215-2227. doi:10.1056/NEJMoa1708538
Pasi KJ, Rangarajan S, Mitchell N, et al. Multiyear Follow-up of AAV5- hFVIII-SQ Gene Therapy for Hemophilia A. New England Journal of Medicine. 2020;382(1):29-40. doi:10.1056/NEJMoa1908490
ClinicalTrials.gov. NIH U.S. National Library of Medicine. https://clinicaltrials.gov/ct2/home. Accessed January 7, 2023.
Kavaklı K, Antmen B, Okan V, et al. Gene therapy in haemophilia: literature review and regional perspectives for Turkey. Ther Adv Hematol. 2022;13:204062072211045. doi:10.1177/20406207221104591
Castaman G, di Minno G, de Cristofaro R, Peyvandi F. The Arrival of Gene Therapy for Patients with Hemophilia A. Int J Mol Sci. 2022;23(18):10228. doi:10.3390/ijms231810228
Colella P, Ronzitti G, Mingozzi F. Emerging Issues in AAV-Mediated In Vivo Gene Therapy. Mol Ther Methods Clin Dev. 2018;8:87-104. doi:10.1016/j.omtm.2017.11.007
Mendell JR, Al-Zaidy SA, Rodino-Klapac LR, et al. Current Clinical Applications of In Vivo Gene Therapy with AAVs. Molecular Therapy. 2021;29(2):464-488. doi:10.1016/j.ymthe.2020.12.007
Wagner HJ, Weber W, Fussenegger M. Synthetic Biology: Emerging Concepts to Design and Advance Adeno-Associated Viral Vectors for Gene Therapy. Advanced Science. 2021;8(9):2004018. doi:10.1002/advs.202004018
High KA, George LA, Eyster ME, et al. A Phase 1/2 Trial of Investigational Spk-8011 in Hemophilia a Demonstrates Durable Expression and Prevention of Bleeds. Blood. 2018;132(Supplement 1):487-487. doi:10.1182/blood-2018-99-115495
Roctavian®. Prescribing information. BioMarin Pharmaceutical, Inc. June 2023. https://d34r3hkxgxjdtw.cloudfront.net/6f836309-d95f- 42af-b717-2efa058ad82d/78bf2bcb-7068-4774-b962- a35c53704fc1/78bf2bcb-7068-4774-b962-
a35c53704fc1_source v.pdf. Accessed September 4, 2023.
Hemgenix®. Prescribing information. uniQure, Inc. November 2022. https://labeling.cslbehring.com/PI/US/Hemgenix/EN/Hemgenix- Prescribing-Information.pdf. Accessed September 4, 2023.
Cantore A, Naldini L. WFH State-of-the-art paper 2020: In vivo lentiviral vector gene therapy for haemophilia. Haemophilia. 2021;27(S3):122-
125. doi:10.1111/hae.14056
Milone MC, O’Doherty U. Clinical use of lentiviral vectors. Leukemia. 2018;32(7):1529-1541. doi:10.1038/s41375-018-0106-0
Jofra Hernández R, Calabria A, Sanvito F, et al. Hematopoietic Tumors in a Mouse Model of X-linked Chronic Granulomatous Disease after Lentiviral Vector-Mediated Gene Therapy. Molecular Therapy. 2021;29(1):86-102. doi:10.1016/j.ymthe.2020.09.030
Schlimgen R, Howard J, Wooley D, et al. Risks Associated With Lentiviral Vector Exposures and Prevention Strategies. J Occup Environ Med. 2016;58(12):1159-1166. doi:10.1097/JOM.0000000000000879
Chen W, Li H, Liu Z, Yuan W. Lipopolyplex for Therapeutic Gene Delivery and Its Application for the Treatment of Parkinson’s Disease. Front Aging Neurosci. 2016;8. doi:10.3389/fnagi.2016.00068
Baru M, Axelrod JH, Nur I. Liposome-encapsulated DNA-mediated gene transfer and synthesis of human factor IX in mice. Gene. 1995;161(2):143-150. doi:10.1016/0378-1119(95)00281-A
Tuddenham E, Ling G, Wolf-Garraway R; The Use of a Pegylated Liposome in a Phase II Trial to Enhance the Potency and Extend the Dosing Interval of Prophylactic Standard Half-Life FVIII, without Increasing the Dose. Blood. 2022;140 (Suppl 1):5586–5587. doi: org/10.1182/blood-2022-170692
Mao HQ, Roy K, Troung-Le VL, et al. Chitosan-DNA nanoparticles as gene carriers: synthesis, characterization and transfection efficiency. J Control Release. 2001;70(3):399-421. doi:10.1016/s0168- 3659(00)00361-8
510(K) Summary HemCon® Bandage. 510(k) K072486. HemCon Medical Technologies, Inc. August 6, 2008. https://www.accessdata.fda.gov/cdrh_docs/pdf7/K072486.pdf. Accessed September 8, 2023.
Okoli G, Hortelano G, Leong K. Oral delivery of plasmid DNA encoding the factor IX gene. Mol Ther. 2000;S28(1).
Nicol F, Wong M, MacLaughlin FC, et al. Poly-L-glutamate, an anionic polymer, enhances transgene expression for plasmids delivered by intramuscular injection with in vivo electroporation. Gene Ther. 2002;9(20):1351-1358. doi:10.1038/sj.gt.3301806
Fewell JG, MacLaughlin F, Mehta V, et al. Gene Therapy for the Treatment of Hemophilia B Using PINC-Formulated Plasmid Delivered to Muscle with Electroporation. Molecular Therapy. 2001;3(4):574-583. doi:10.1006/mthe.2001.0295
Gharwan H, Wightman L, Kircheis R, Wagner E, Zatloukal K. Nonviral gene transfer into fetal mouse livers (a comparison between the cationic polymer PEI and naked DNA). Gene Ther. 2003;10(9):810-817. doi:10.1038/sj.gt.3301954
Jinturkar KA, Rathi MN, Misra A. Gene Delivery Using Physical Methods. In: Challenges in Delivery of Therapeutic Genomics and Proteomics. Elsevier; 2011:83-126. doi:10.1016/B978-0-12-384964-9.00003-7
Miao CH. A Novel Gene Expression System: Non-Viral Gene Transfer for Hemophilia as Model Systems. In: 2005:143-177. doi:10.1016/S0065- 2660(05)54007-0
Li R, Wang Q, She K, Lu F, Yang Y. CRISPR/Cas systems usher in a new era of disease treatment and diagnosis. Molecular Biomedicine. 2022;3(1):31. doi:10.1186/s43556-022-00095-y
Jinek M, Chylinski K, Fonfara I, Hauer M, Doudna JA, Charpentier E. A Programmable Dual-RNA–Guided DNA Endonuclease in Adaptive Bacterial Immunity. Science (1979). 2012;337(6096):816-821. doi:10.1126/science.1225829
Gaj T, Gersbach CA, Barbas CF. ZFN, TALEN, and CRISPR/Cas-based methods for genome engineering. Trends Biotechnol. 2013;31(7):397-
405. doi:10.1016/j.tibtech.2013.04.004
Adachi H, Hengesbach M, Yu YT, Morais P. From Antisense RNA to RNA Modification: Therapeutic Potential of RNA-Based Technologies. Biomedicines. 2021;9(5):550. doi:10.3390/biomedicines9050550
Li H, Haurigot V, Doyon Y, et al. In vivo genome editing restores haemostasis in a mouse model of haemophilia. Nature. 2011;475(7355):217-221. doi:10.1038/nature10177
Davidoff AM, Nathwani AC. Genetic Targeting of the Albumin Locus to Treat Hemophilia. New England Journal of Medicine. 2016;374(13):1288-1290. doi:10.1056/NEJMcibr1600347
ClinicalTrials.gov Identifier: NCT02695160. U.S. National Library of Medicine. Ascending Dose Study of Genome Editing by Zinc Finger Nuclease Therapeutic SB-FIX in Subjects with Severe Hemophilia B. Published June 28, 2021. https://clinicaltrials.gov/ct2/show/NCT02695160?term=NCT02695160& draw=2&rank=1. Accessed January 9, 2023.
Pasi KJ, Rangarajan S, Georgiev P, et al. Targeting of Antithrombin in Hemophilia A or B with RNAi Therapy. New England Journal of Medicine. 2017;377(9):819-828. doi:10.1056/NEJMoa1616569
Wang L, Yang Y, Breton CA, et al. CRISPR/Cas9-mediated in vivo gene targeting corrects hemostasis in newborn and adult factor IX–knockout mice. Blood. 2019;133(26):2745-2752. doi:10.1182/blood.2019000790
Chuang YF, Phipps AJ, Lin FL, et al. Approach for in vivo delivery of CRISPR/Cas system: a recent update and future prospect. Cellular and
Molecular Life Sciences. 2021;78(6):2683-2708. doi:10.1007/s00018- 020-03725-2
Lambert T, Benson G, Dolan G, et al. Practical aspects of extended half- life products for the treatment of haemophilia. Ther Adv Hematol. 2018;9(9):295-308. doi: 10.1177/2040620718796429
Maestro S, Weber ND, Zabaleta N, Aldabe R, Gonzalez-Aseguinolaza G. Novel vectors and approaches for gene therapy in liver diseases. JHEP Rep. 2021;3(4):100300. doi: 10.1016/j.jhepr.2021.100300
Nathwani AC. Gene therapy for hemophilia. Hematology Am Soc Hematol Educ Program. 2019;2019(1):1-8. doi: 10.1182/hematology.201900000
Monahan PE, Négrier C, Tarantino M, Valentino LA, Mingozzi F. Emerging Immunogenicity and Genotoxicity Considerations of Adeno- Associated Virus Vector Gene Therapy for Hemophilia. J Clin Med. 2021;10(11):2471. doi: 10.3390/jcm10112471
Park CY, Lee DR, Sung JJ, Kim DW. Genome-editing technologies for gene correction of hemophilia. Hum Genet. 2016;135(9):977-81. doi: 10.1007/s00439-016-1699-x
Antihemophilic Factor (Human) (Monograph). ASHP. February 24, 2023. https://www.drugs.com/monograph/antihemophilic-factor-human.html. Accessed September 1, 2023.
Arruda VR, Samelson-Jones BJ. Obstacles and future of gene therapy for hemophilia. Expert Opin Orphan Drugs. 2015;3(9):997-1010. doi:10.1517/21678707.2015.1069179
Hermans C, Gruel Y, Frenzel L, Krumb E. How to translate and implement the current science of gene therapy into haemophilia care?. Ther Adv Hematol. 2023;14:20406207221145627. Published 2023 Jan
12. doi:10.1177/20406207221145627
DISCLAIMER
The information provided in this course is general in nature, and it is solely designed to provide participants with continuing education credit(s). This course and materials are not meant to substitute for the independent, professional judgment of any participant regarding that participant’s professional practice, including but not limited to patient assessment, diagnosis, treatment, and/or health management. Medical and pharmacy practices, rules, and laws vary from state to state, and this course does not cover the laws of each state; therefore, participants must consult the laws of their state as they relate to their professional practice.
Healthcare professionals, including pharmacists and pharmacy technicians, must consult with their employer, healthcare facility, hospital, or other organization, for guidelines, protocols, and procedures they are to follow. The information provided in this course does not replace those guidelines, protocols, and procedures but is for academic purposes only, and this course’s limited purpose is for the completion of continuing education credits.
Participants are advised and acknowledge that information related to medications, their administration, dosing, contraindications, adverse reactions, interactions, warnings, precautions, or accepted uses are constantly changing, and any person taking this course understands that such person must make an independent review of medication information prior to any patient assessment, diagnosis, treatment and/or health management. Any discussion of off-label use of any medication, device, or procedure is informational only, and such uses are not endorsed hereby.
Nothing contained in this course represents the opinions, views, judgments, or conclusions of RxCe.com LLC. RxCe.com LLC is not liable or responsible to any person for any inaccuracy, error, or omission with respect to this course, or course material.
© RxCe.com LLC 2023: All rights reserved. No reproduction of all or part of any content herein is allowed without the prior, written permission of RxCe.com LLC.
